Glucagon-like peptide-1 (GLP-1) weight loss drugs have become quite popular for those who are living with diabetes, obesity, or both. According to research, GLP-1 weight loss drugs can also be beneficial for those with sleep apnea or symptoms of heart failure. The drugs have a positive impact on patients’ health and could potentially be beneficial for other conditions, which is how they’ve become so widespread.
Glucagon-like peptide-1 (GLP-1) weight loss drugs have become quite popular for those who are living with diabetes, obesity, or both. According to research, GLP-1 weight loss drugs can also be beneficial for those with sleep apnea or symptoms of heart failure. The drugs have a positive impact on patients’ health and could potentially be beneficial for other conditions, which is how they’ve become so widespread.
Many employers recognize the potential of GLP-1 weight loss drugs and how they’re making an impact on their employees’ lives. As research on GLP-1s continues to grow and their use expands to additional conditions, more individuals may benefit. This makes it essential for employers to consider how to incorporate GLP-1s into their health plans as their use becomes more widespread.
According to an International Foundation of Employee Benefit Plans (IFEBP) survey report, approximately one-third of employer health plans cover GLP-1s for both diabetes and weight loss, which is up from 26 percent in 2023. While this number is rising, many employers are wondering how to integrate GLP-1s into their health plans.
Why There’s a Demand for GLP-1s
As the popularity of GLP-1 weight loss drugs has increased, so too has the demand from employees for the drugs to be covered, and understandably so. GLP-1 weight loss drugs can help people lose 15-20 percent of their body weight, reduce their risk of other health conditions arising from obesity, and improve their quality of life.
However, these drugs come with a steep cost. Without insurance and rebates, GLP-1s can cost employees around $1,000 a month before insurance and rebates.
It’s clear that these drugs can have a profound impact on patients’ lives, including enhancing their quality of life and reducing medical costs that can arise from chronic conditions related to obesity. In turn, these reduced costs can benefit employers.
How should they address the costs associated with covering GLP-1s, and moreover, how should they integrate them into their health plan?
How to Integrate GLP-1 Weight Loss Drugs into a Health Plan
One of the largest decisions employers need to make is whether to cover GLP-1s for diabetes only or to cover both diabetes and weight management. About 57 percent of health plans cover GLP-1s for diabetes but not weight management, and 19 percent of these employers are considering covering them for weight management, the IFEBP survey report found.
Employers also need to determine which strategies they’ll implement to cover these drugs while keeping benefits costs reasonable for all employees. Here are some strategies that employers can implement to integrate GLP-1s into their health plans:
Formulary Adjustment
Considering how much GLP-1s cost, employers must work with benefits advisors and pharmacy consultants to prioritize the highest-value medications and ensure the most effective treatments are available to employees. Then, employers should periodically review members’ health outcomes and continue to make adjustments to the formulary to include more cost-effective medications as they become available. This strategy helps employers ensure their formulary aligns with their own financial goals and their employees’ health goals.
Some employers also take this strategy a step further and incorporate several strategies. For example, they may adjust the formulary while incorporating prior authorization or lifestyle management strategies.
Proactive Drug Utilization Management
GLP-1s have been shown to be beneficial for weight management, but it can also be easy to abuse them for purposes such as crash dieting, which could drive up costs and diminish the available supply for those who truly need them.
A few strategies to help curb unnecessary utilization include:
- Requiring prior authorization to ensure the drug is used for approved purposes
- Implementing step therapy for employees to try less expensive drugs before they can access more expensive ones
- Requiring GLP-1s be prescribed to those who may benefit from them the most
- Establishing quantity limits with 30-day supplies of GLP-1s because larger prescriptions may be wasteful if a person stops taking them
Lifestyle Intervention Programs
GLP-1 weight loss drugs are generally not effective on their own. Research indicates that physical activity and dietary changes are essential components of improving the efficacy of GLP-1 weight loss drugs.
Employers should ensure weight loss solutions integrate with existing weight management, hypertension, and diabetes programs. These solutions should be centered on nutritional support and exercise guidance. Members in the program should be followed closely and supported throughout their weight loss journey. The goal of these programs should be to take a member off of GLP-1s after losing weight if they don’t require it for an underlying condition.
Even employees who may be at risk for a condition but are otherwise healthy can benefit from lifestyle programs focused on prevention. For those who are already taking medication for a condition, a prevention program can help reduce comorbidities that could lead to high pharmacy costs.
Alternative Sourcing Arrangement
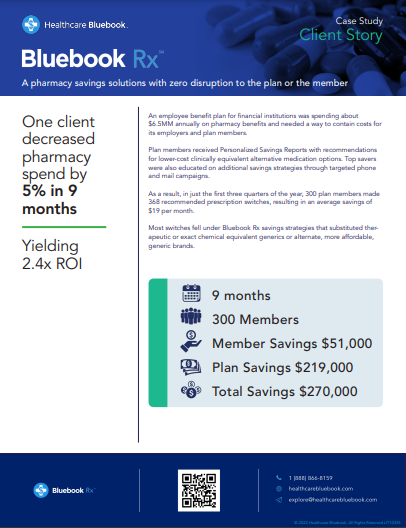
Alternative prescription sourcing arrangements can ensure employees have what they need while reducing costs. Programs such as Bluebook Rx can help reduce pharmacy spend by sourcing alternatives and continuously monitoring for additional ways to save.
Bluebook Rx evaluates claims data to see where overpriced medications are being used. Then, the program sends a personalized report to members containing recommendations for comparable, lower-cost alternatives. Members also have access to a licensed pharmacy team for personalized guidance.
Bluebook Rx has expanded with an innovative GLP-1 savings program, which is focused on reducing the cost of GLP-1s. The expansion enables members and employers to drastically reduce their GLP-1 pharmacy costs, which enables members to still receive their necessary medications while factoring in costs.
Ready to Save on GLP-1s and Other Medications?
It’s critical to ensure employees have the medications they need for their health and well-being, but it’s also essential to consider costs. Healthcare Bluebook’s powerful pharmacy savings program, Bluebook Rx, now bolstered by our partnership with Vālenz Health®, ensures employers can do both.
Explore our Bluebook Rx case study to see how other organizations have reduced their pharmacy spend.